Apixaban and edoxaban are anticoagulant drugs employed for the prevention of blood clot formation and stroke.
Their reduction in patients diagnosed with specific medical conditions, such as atrial fibrillation (an irregular heart rhythm) or venous thromboembolism (blood clots in the veins).
Locally, edoxaban is the favored anticoagulant of choice, as it offers several advantages for your local NHS.
Moreover, opting for edoxaban over other anticoagulants enables the healthcare system to cater to a larger number of patients.
This is attributed to the fact that two patients can receive treatment with edoxaban for the same resources. It required treating only one patient with an alternative anticoagulant.
Why Change From Apixaban To Edoxaban?
The decision to transition from apixaban to edoxaban or another medication can differ based on individual patient circumstances. Several potential factors for switching between DOACs (Direct Oral Anticoagulants) may encompass:
Efficacy and Tolerability:
One drug may work better for a particular patient in terms of preventing blood clots or have fewer side effects.
Cost and Insurance Coverage:
Some patients may need to switch medications due to changes in their insurance coverage or medication costs.
Drug Interactions:
If a patient starts taking a new medication that interacts with apixaban but not edoxaban, a switch may be necessary.
Renal Function:
Certain DOACs are eliminated from the body through the kidneys, and their use may need to be adjusted in patients with impaired kidney function.
Patient Preference:
In some cases, patients may prefer to take one medication over another due to factors like dosing frequency or other personal considerations.
New Medical Evidence:
Occasionally, new research or clinical trials may reveal differences in the safety or effectiveness of one medication over another, leading to changes in prescribing practices.
Dosing Regimen:
The dosing frequency and schedule of apixaban and edoxaban may differ. Some patients may find it more convenient to take one medication over the other based on their lifestyle and daily routine.
Bleeding Risk:
Both apixaban and edoxaban are associated with a risk of bleeding. Which is a potential side effect of anticoagulant therapy. The decision to switch medications might be influenced by a patient’s bleeding risk profile.
Previous Adverse Events:
If a patient experiences adverse events or side effects with one medication, a switch to another DOAC might be considered to see if the new medication is better tolerated.
Drug Availability:
Availability of medications can vary based on geographic location or other factors. In some cases, a switch might be necessitated by the availability of a specific medication.
Patient Compliance:
Some patients may struggle with adherence to their prescribed medication regimen. Switching to a different medication might be attempted to improve compliance if other interventions have not been successful.
Clinical Guidelines:
Changes in clinical guidelines or recommendations from medical societies might influence the choice of anticoagulant therapy for certain conditions, which could lead to a switch in medications.
Transitioning from Apixaban to Edoxaban in Anticoagulant Therapy
Here is a resource, where you get more information and understand the key aspects of transitioning from Apixaban to Edoxaban, shedding light on the potential advantages, challenges, and important clinical considerations.
What factors should be considered when selecting the appropriate anticoagulant therapy?
Apixaban and Edoxaban are both oral anticoagulant medications. It is used to prevent and treat thromboembolic disorders. Additionally, These drugs belong to the class of direct oral anticoagulants (DOACs).
Which are increasingly preferred over traditional Vitamin K antagonists like warfarin due to their predictable pharmacokinetics and simplified dosing regimens. Here’s a brief overview of each medication:
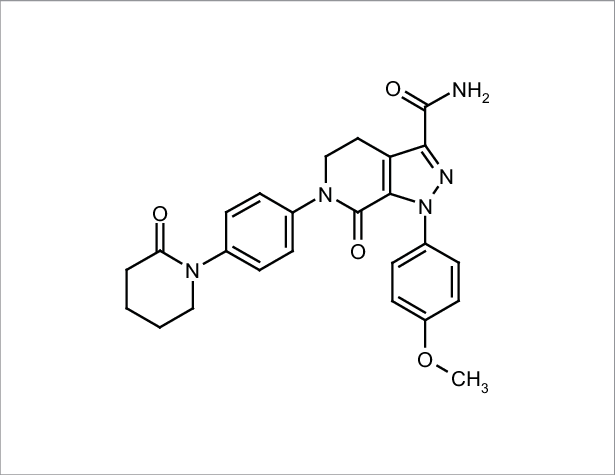
Apixaban:
- Mechanism of Action: Apixaban is a selective and reversible inhibitor of Factor Xa, an essential coagulation protein.
By targeting Factor Xa, Apixaban interrupts the coagulation cascade and prevents the formation of blood clots.
- Indications: Apixaban is primarily indicated for the prevention of stroke and systemic embolism in patients.
It works with non-valvular atrial fibrillation (NVAF) and for the treatment and prevention of deep vein thrombosis (DVT) and pulmonary embolism (PE).
- Dosage: The recommended dose of Apixaban may vary.It depends on the indication and patient characteristics. Common doses include 2.5 mg or 5 mg taken orally twice daily.
Edoxaban:
- Mechanism of Action: Edoxaban is also a selective and reversible inhibitor of Factor Xa, similar to Apixaban. It prevents blood clot formation by inhibiting Factor Xa’s activity.
- Indications: Edoxaban is used for the prevention of stroke and systemic embolism in patients with NVAF, treatment of DVT and PE, and prophylaxis of VTE following hip or knee replacement surgery.
- Dosage: Edoxaban is typically available in doses of 15 mg or 60 mg taken orally once daily, with variations based on patient factors and indication.
Comparing Apixaban and Edoxaban:
- Firstly, both Apixaban and Edoxaban have demonstrated efficacy and safety profiles in various clinical trials. They make them viable options for anticoagulation therapy.
- Secondly, the dosing regimens differ, with Apixaban requiring twice-daily administration and Edoxaban requiring once-daily dosing. Which may influence patient adherence and convenience.
- Thirdly, renal function plays a crucial role in the choice of anticoagulant, as Apixaban’s excretion is primarily renal, whereas Edoxaban has a dual elimination route (renal and hepatic).
- Finally, drug interactions may vary between the two medications, and healthcare providers should consider a patient’s concomitant medications before selecting the appropriate anticoagulant.
What are the key clinical factors and challenges to be mindful of when transitioning between anticoagulant therapies?
The decision to change from one anticoagulant to another should be guided by patient-specific characteristics and individual risk-benefit assessments. Here’s an overview of the key clinical considerations for changing anticoagulants:
Patient-Specific Factors:
- Age and Weight: Age-related changes in metabolism and drug clearance, as well as weight fluctuations, can impact the pharmacokinetics of anticoagulants.
- Renal Function: The kidney plays a crucial role in excreting many anticoagulants. It impaired renal function can affect drug clearance. It leads to an increased risk of bleeding or reduced efficacy.
- Liver Function: Anticoagulants that undergo hepatic metabolism.It may require dose adjustments in patients with liver impairment.
- Drug Interactions: Potential interactions with other medications the patient is taking should be assessed to avoid adverse effects or altered anticoagulant efficacy.
What are the medical reasons that might lead to a decision to change anticoagulant therapies?
- Inadequate Efficacy: If the current anticoagulant fails to provide the desired therapeutic effect, switching to an alternative with better efficacy may be considered.
- Adverse Effects or Allergic Reactions: Patients experiencing intolerable side effects or allergic reactions to the current anticoagulant may necessitate a change to a different agent.
- Medication Adherence: Poor adherence to the prescribed anticoagulant regimen may prompt a switch to a medication with a more convenient dosing schedule or administration route.
- New Clinical Indications: Changes in the patient’s medical condition or the development of new clinical indications may warrant a switch to a more suitable anticoagulant.
- Renal Impairment: Decline in renal function may necessitate. It changes to an anticoagulant with reduced renal excretion to prevent drug accumulation and potential bleeding complications.
- Comparative Safety and Efficacy: Evaluate head-to-head clinical trials and real-world evidence comparing the safety and efficacy of the current and proposed anticoagulants.
- Duration of Anticoagulation: Assess the intended duration of anticoagulation therapy, as this can influence the choice of anticoagulant and the risk-benefit profile.
What are the factors that healthcare professionals should take?

Switching or transitioning from one anticoagulant to another requires careful planning and consideration to ensure patient safety and efficacy of the new medication.
In addition, several factors need to be taken into account during the switch, including timing, dosing considerations, potential drug interactions, and monitoring for any adverse effects.
Read More about Mental Health
Timing of Switch
The timing of the switch is crucial to ensure continuity of anticoagulation and prevent a gap in therapy.
Moreover, healthcare providers should consider the pharmacokinetics of the current anticoagulant and the new medication to determine the optimal timing for the switch.
Dosage Considerations: Dosage adjustments may be necessary when transitioning from one anticoagulant to another, especially if the medications have different potencies or clearance rates.
Drug Interactions: Potential drug interactions between the current and new anticoagulants, as well as interactions with other medications the patient is taking, should be carefully evaluated.
Additionally, avoiding harmful drug interactions is essential to prevent adverse effects or altered anticoagulant efficacy.
Starting the New Anticoagulant: Initiating the new anticoagulant should be done with careful consideration of the patient’s medical condition and the intended therapeutic indication.
Healthcare providers must ensure the patient receives the correct starting dose and instructions for continued use.
FAQs
Why is edoxaban better than apixaban?
The statement “Edoxaban is better than Apixaban” is subjective and requires context. Both Edoxaban and Apixaban are direct oral anticoagulants (DOACs) with proven efficacy and safety profiles.
Is edoxaban safer than apixaban?
Both Edoxaban and Apixaban are considered safe and effective direct oral anticoagulants (DOACs) with similar bleeding and thromboembolic risk profiles. The safety of each medication depends on individual patient characteristics, medical history, and specific clinical indications.
How do I switch between apixaban and edoxaban?
Switching from Apixaban to Edoxaban should be done under the guidance of a healthcare professional.
The process involves determining the appropriate timing, dosage adjustment, and monitoring to ensure a smooth and safe transition between the two anticoagulant medications.
What are the advantages of edoxaban?
Edoxaban has several advantages. It includes once-daily dosing, a predictable pharmacokinetic profile, and a reduced risk of major bleeding compared to warfarin in certain patient populations.
What are the disadvantages of edoxaban?
The disadvantages of edoxaban include a higher risk of gastrointestinal bleeding compared to warfarin in certain patient populations and the lack of a specific reversal agent. Which may be a concern in emergency situations.
What is the most common risk of edoxaban?
The disadvantages of edoxaban include a higher risk of gastrointestinal bleeding compared to warfarin in certain patient populations and the lack of a specific reversal agent, which may be a concern in emergency situations.
Is edoxaban safer than rivaroxaban?
There is no definitive evidence to suggest that Edoxaban is universally safer than Rivaroxaban. Both medications are direct oral anticoagulants (DOACs) with similar safety profiles.
The choice between the two should be based on individual patient characteristics and clinical considerations.
Which is more expensive edoxaban or apixaban?
The cost of Edoxaban and Apixaban may vary depending on factors such as location, insurance coverage, and the specific formulation.
Generally, the cost of Edoxaban tends to be slightly higher than Apixaban. However, it is essential to check current pricing and consult with a healthcare provider or pharmacist for the most accurate and up-to-date information
Conclusion
The decision to change from one anticoagulant to another should be based on a careful assessment of patient-specific factors, clinical considerations, and comparative evidence.
Additionally, healthcare providers must take into account the patient’s age, weight, renal and liver function, and potential drug interactions when considering a switch.
Reasons for changing anticoagulants may include inadequate efficacy, adverse effects, medication adherence issues, or new clinical indications. Moreover, comparative studies and clinical trials offer valuable insights into the safety and efficacy of different anticoagulants, aiding in informed decision-making.
Switching protocols should be followed meticulously. It considers timing, dosing adjustments, drug interactions, and monitoring during the transition.
Proper patient education and counseling are vital to ensure compliance and safety with the new anticoagulant therapy. Patient preferences and shared decision-making play a crucial role in optimizing treatment outcomes.
Decision-making and an evidence-based approach are essential in selecting the most appropriate anticoagulant for each patient. By navigating the switch with caution and diligence, healthcare providers can improve patient outcomes and enhance the quality of anticoagulation therapy.